Struggling With Reflux Either Before Or After Surgery?
Gastroesophageal reflux (aka- heartburn) is very common in the weight loss surgery community. GERD results from content in the stomach refluxing up into the throat, causing heartburn and regurgitation. Roughly 55% of those who with obesity have GERD.
There is significant variability among surgeons in terms of pre-operative work-up for GERD. If you’ve struggled with reflux prior to surgery, your surgeon may do some, all, or none of the following things prior to bariatric surgery:
- Complete a questionnaire (called a GERD Q1 Survey) to evaluate the clinical severity of your symptoms.
- Perform a swallow study (known as an Upper GI). This imaging study can detect important anatomy variations in the esophagus, can identify reflux, hiatal hernias, and the functionality of how the esophagus coordinates swallowing.
- Perform a procedure known as an EGD (“esophagogastroduodenoscopy”, otherwise known as an upper endoscopy). In this procedure, the surgeon uses a camera to look down the esophagus, stomach, and early part of the small intestine. The purpose is to examine the anatomy and lining of each of these areas.
- pH studies – used as an adjunct to help diagnose GERD in patients who may not have significant symptoms
- Esophageal manometry
The laparoscopic sleeve gastrectomy is the most commonly performed bariatric surgery in the US and comprises 60% of all cases. The topic over the development of new onset reflux after this procedure and worsening GERD symptoms in patients with pre-existing reflux continues to remain a controversial topic.
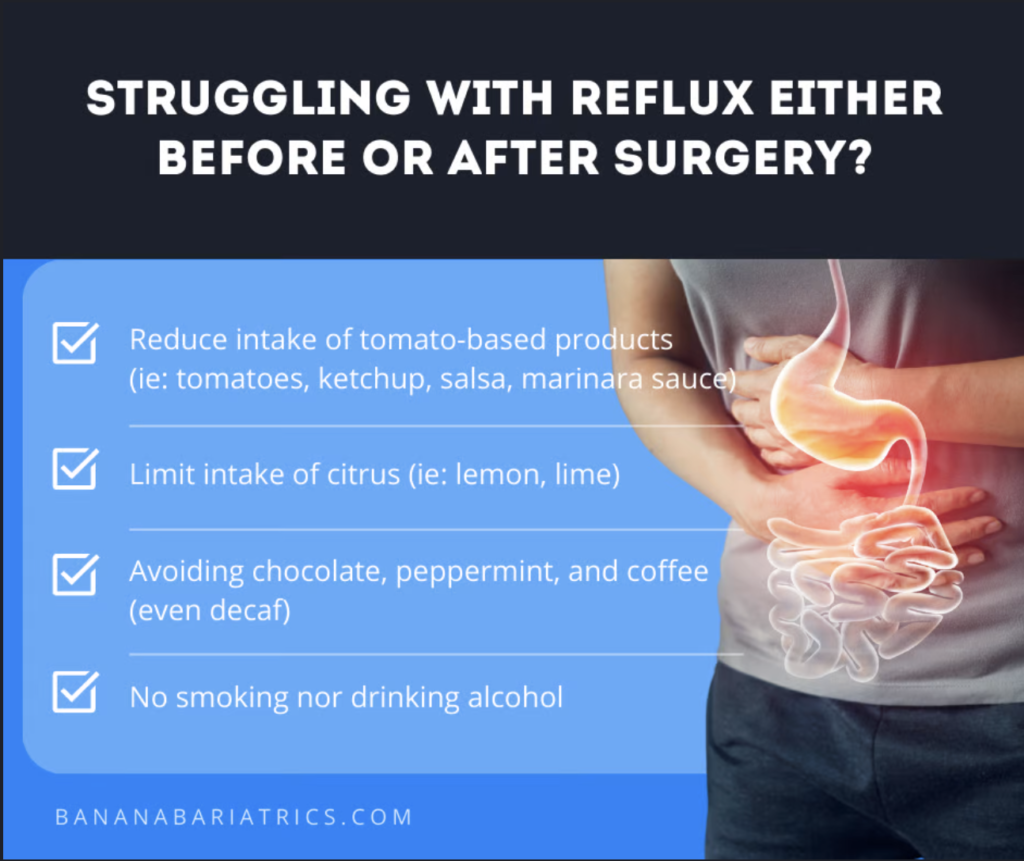
If you have had surgery and are struggling with reflux, start with some of the basic dietary modifications (watch our Instagram Reel on acid reflux):
- Reducing intake of tomato-based products (ie: tomatoes, ketchup, salsa, marinara sauce)
- Limiting intake of citrus (ie: lemon, lime)
- Avoiding chocolate, peppermint, and coffee***
- No smoking nor drinking alcohol
***When it comes to coffee, even decaf coffee can contribute to GERD. However, you can try purchasing low acidic coffee online as an approach to improve reflux symptoms.
Other lifestyle modifications you can try are waiting at least 3-4 hours after eating before lying down for bed in addition to sleeping with your head of bed elevated at least 30 degrees at night (on a few pillows).
As you continue to progress in your weight loss surgery journey, weight loss can actually help reduce GERD symptoms.
However, if diet and lifestyle changes are ineffective, the next step is to take an acid-reducing medication. If these medications fail to work, there are more invasive endoscopic procedures that your surgeon and/or gastroenterologist can discuss with you.
The last option for management of reflux after surgery is a revision to the Roux en Y Gastric Bypass (RYGB) procedure. Resolution of GERD symptoms have been reported to be ~65% in patients who undergo a revision from a sleeve gastrectomy to RYGB.
While this statistic is reassuring, there have been other studies that have shown persistent reflux symptoms in 22% of patients- despite undergoing a revision to RYGB.
If you had had a revision to RYGB and are still experiencing reflux symptoms despite implementation of everything listed above, your surgeon and/or GI specialist may still have additional surgical revisional options they can discuss with you in order to help control your GERD symptoms.
Bibliography: King, Keith, et al. “Assessment and Management of Gastroesophageal Reflux Disease Following Bariatric Surgery.” Surgery for Obesity and Related Diseases, vol. 17, no. 11, 2021, pp. 1919–1925., https://doi.org/10.1016/j.soard.2021.07.023.
Was this information helpful?
We have a whole library vault full of bariatric specific education as well as informational courses on Nutrition, Mindfulness, and getting back on track after weight loss surgery. All of this is tucked inside our exclusive membership support group, Banana Bariatrics.
Come and join us on “the inside”!
Share with others:
JOIN OUR COMMUNITY:



Responses